News Story
Fighting Fungus: Engineering Antibodies for Validating Antifungal Drug Targets

Assistant Professor Amy Karlsson (Department of Chemical and Biomolecular Engineering).
Bacterial infections are not the only drug-resistant illnesses. Candidiasis, typically caused by the C. albicans fungus, is one of the most common hospital-acquired bloodstream infections. Also known as a yeast infection, localized candidiasis of the skin, mouth, nails and other parts of the body are often easily treated. In immunocompromised patients, however, the infection may spread throughout the body, evolving into a life-threatening form of sepsis called candidemia. C. albicans’ combination of natural and increasingly acquired drug-resistance has led the CDC to declare the fungus a “serious threat” to human health.1
Amy Karlsson, an assistant professor in the University of Maryland’s Department of Chemical and Biomolecular Engineering, is developing a new process that more accurately simulates the effect of antifungal drugs on their targets, which she believes will convert more discoveries in the lab into products on the shelf. Karlsson recently received a Ralph E. Powe Junior Faculty Enhancement Award from Oak Ridge National Laboratory to support the project.
In the search for new antifungal drugs, researchers try to identify the proteins and cellular functions that affect a fungus’ virulence and health, as well as the genes responsible for controlling them. Drugs are then designed to attack these targets. Although many targets have been discovered, very few new antifungal agents have been successful. Karlsson and her research group believe this is because the way in which the targets are disabled in the lab is unrelated to the way antifungal drugs do so in the body.
Potential targets are typically identified using a procedure known as gene knockout, in which a gene is removed to determine what effect it has on an organism’s behavior. If removing a gene from C. albicans eliminates the production of a protein responsible for virulence, that protein is identified as a possible drug target.
“When a gene knockout is used, the protein encoded by the gene is also eliminated,” Karlsson explains. “But when an antifungal drug is used to inhibit a protein target, it doesn’t remove the protein from the cell. It binds to the protein and disrupts its cellular function. Knocking out the gene tells us what to attack, but not how.”
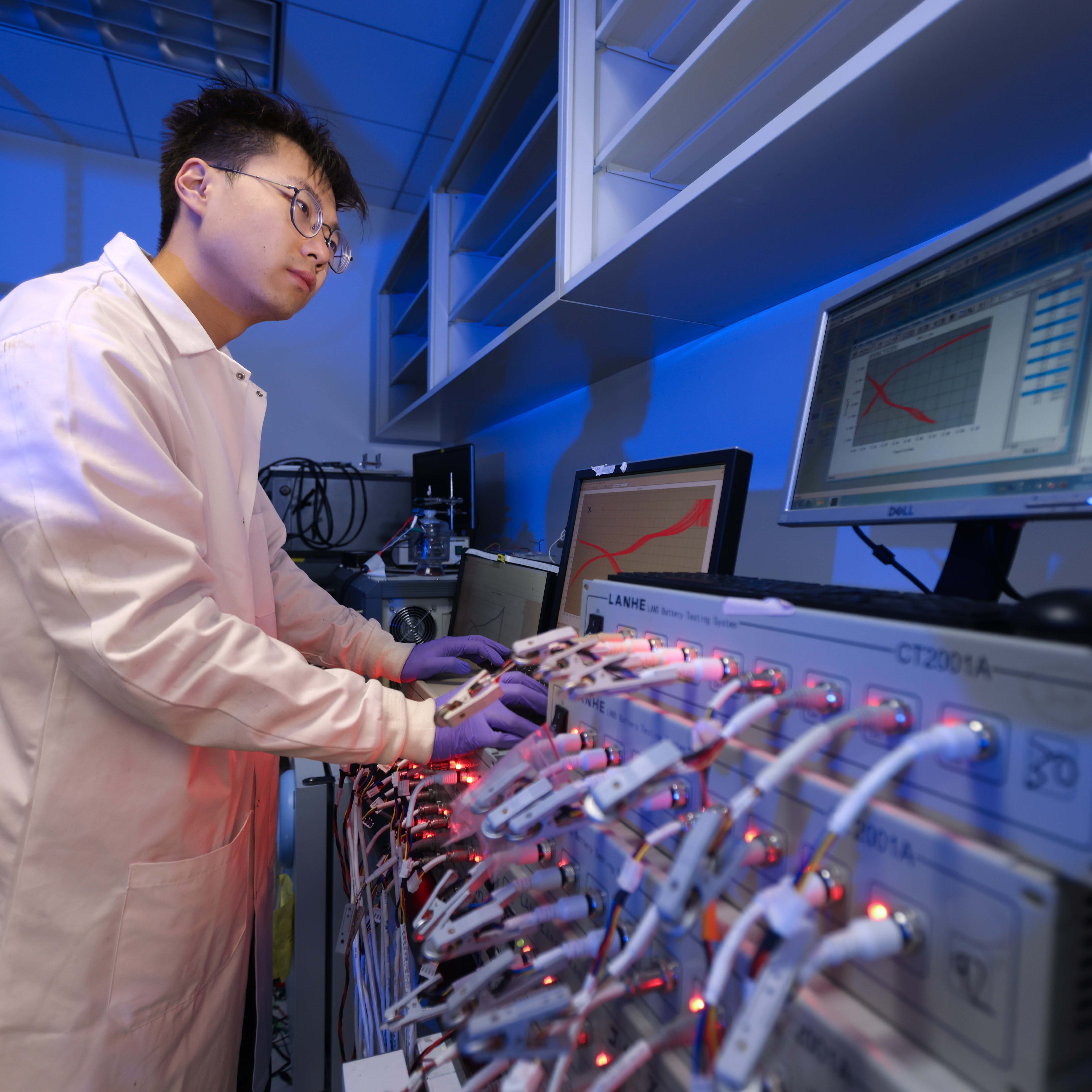
The Karlsson Group’s novel approach is to focus on the proteins instead of the encoding genes that produce them. The team’s strategy is to mimic the behavior of antifungal drugs by using engineered antibodies that disrupt the function of potential antifungal drug targets at the protein level.
After engineering an antibody that binds to the target protein, Karlsson and her team need to get it into the C. albicans cells. Drug delivery is difficult under normal circumstances, and this simulated drug delivery is even more challenging because antibodies are not naturally evolved to work within cells.
Karlsson and her group are addressing this problem by evolving intrabodies, antibodies capable of functioning inside of a cell, in the lab. They then prompt C. albicans to produce these intrabodies on its own, bypassing the need to develop a drug delivery system to get the intrabodies into cells.
“Our intrabodies disable both the target protein and the activities it performs, so we can identify exactly what that protein does and which of its parts enable the pathogen to survive and to affect us,” Karlsson explains. “If we used gene knockouts, we probably wouldn’t be able to observe that.” And, she adds, the technique can be used to study proteins in any type of cell, making it an efficient and effective tool for biomolecular research.
“This project will develop a powerful new drug target validation tool for C. albicans and provide biochemical information that will guide drug design,” says Karlsson. “We may even identify engineered antibodies that could serve as therapeutics themselves.”
1 Centers for Disease Control and Prevention (2013). Antibiotic Resistance Threats in the United States, 2013. Retrieved September 18, 2013, from www.cdc.gov/drugresistance/threat-report-2013/.
Published August 18, 2014